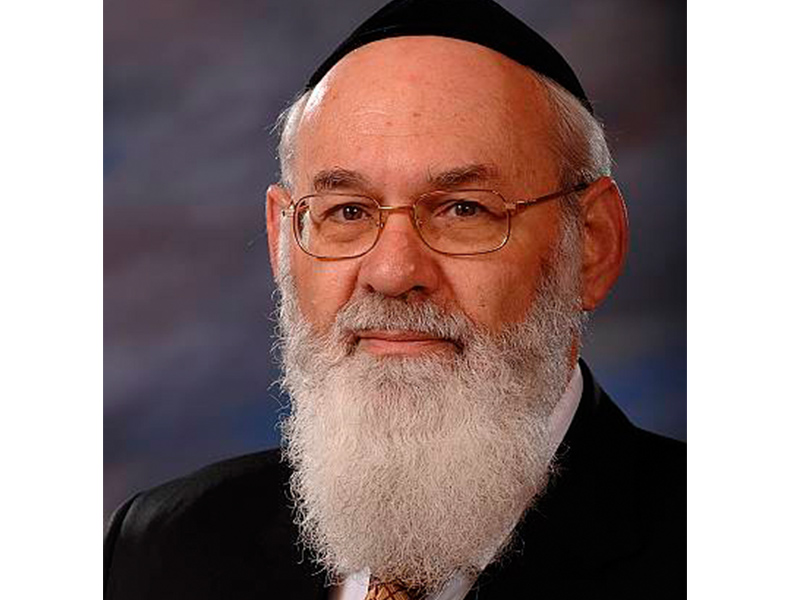
Rabbi Avraham Steinberg is a senior pediatric neurologist at Shaare Zedek Medical Center in Jerusalem and director of the hospital’s medical ethics unit. He is also an associate clinical professor of medical ethics at Hebrew University Hadassah Medical School.
In the early 2000s, Rabbi Steinberg headed the committee that drafted Israel’s Dying Patient Law, which passed in 2005. Last month, Rabbi Steinberg was in Ottawa to speak at Torah in Motion’s Jewish Medical Ethics conference. He subsequently gave a talk in Toronto about end-of-life issues, also hosted by Torah in Motion.
How did you come to head the committee that drafted Israel’s Dying Patient Law?
I’ve long been involved with a lot of legislation and rabbinic authority concerning health-care issues. In 2000, there was a big controversy in Israel about whether you’re allowed to withdraw a respirator from an ALS patient. There was no law at that time defining what you do concerning a dying patient. Doctors would act according to what they individually thought was right. There was no uniformity on how to treat a patient that is dying.
The controversy created an opportunity for creating legislation. The minister of health asked me to head the committee in charge of drafting it.
What did your committee’s process entail?
The process took us about two years. I knew this was an issue that involved a lot of emotion and different opinions. People differ in opinions on this based on their professional background and ideological background. And in Israel, we don’t just have Jews, but Christians, Muslims and Druze. I thought consultations should be as wide as possible and the committee should then come to some kind of consensus.
So after deliberating, I came up with the idea of forming a committee large enough to divide into four sub-committees according to professional background. These were 1) the medical-scientific sub-committee, which included physicians who deal with dying patients directly, as well as nurses and social workers; 2) the legal sub-committee, which included judges, lawyers, professors of law and academics; 3) the philosophical-ethical sub-committee, which included ethicists and religious leaders from non-Jewish backgrounds; and 4) the Jewish law sub-committee, which included rabbis and physicians who are experts in the field.
I gave each of the four sub-committees the task of coming up with a piece of legislation that covered the major issues that needed to be addressed. So then I got four different suggested pieces of legislation and had to work to put them together and create as wide a consensus as possible.
In general, I think we ultimately wrote a nice piece of legislation and submitted it to the government, who gave it to the Knesset. There were then close to two years of deliberations in the Knesset. Finally, the government introduced legislation that wasn’t far off from what my committee had suggested. That was enacted in 2005 and is now the law in Israel.
What are the law’s main principles?
It contains about 150 paragraphs. It’s hard to summarize it in a short telephone conversation. But it’s certainly different from laws in other places in the world, because of Israel’s character as a Jewish and democratic state. And actually, there was no debate between the different religious representatives in Israel on the law. The debate that existed was between the religious and the non-religious representatives.
Anyways, the major issue was the weight that the secular world gives to a patient’s autonomy as opposed to the value of life compared to the weight the religious world gives to value of life versus autonomy. In a secular state like the United States and probably also Canada, autonomy is the overriding principle. If a patient doesn’t want to live, then in various circumstances, you have to go with that. The interpretation in the secular world seems to be that withdrawing a respirator is not an act of killing.
But the question for everyone still is: where do you draw the line between autonomy and value of life? Every country I know of in the world is trying to strike a balance between these somehow, and different countries draw the line in different places.
So where does Israel draw this line?
Israel respects both autonomy and value of life. So in order to find a middle way between the two, we say the following: if a patient is dying – meaning he fits the definition of dying we’ve set – and he doesn’t want to live and he says ‘Let me die of my illness,’ we respect his autonomy, despite the fact we could prolong his life with medical intervention. That means we won’t do anything active to prolong his life. But also, we don’t allow doing anything active that causes the death of the patient. We don’t allow active euthanasia and we don’t allow physician-assisted
suicide.
We allow the withholding of treatment, but we don’t allow the withdrawing of treatment.
How do you define the difference between withholding and withdrawing?
Let’s say a person is getting dialysis. He gets dialysis on Tuesday and he’s supposed to come back on Friday for another round, but he decides he doesn’t want to. We allow him to stop, because this is a new round of treatment and is considered withholding treatment. That’s OK under the law.
But say a person is using a pacemaker. That’s continuous treatment. So if he stops it, he’ll be dead. If you take away a person’s pacemaker, it’s the same as active euthanasia. So it’s not allowed under the law.
Another example: chemotherapy is an intermittent treatment, not continuous. So a patient can do a few rounds of it and then decide he doesn’t want to do more rounds. That’s fine. We don’t make him get more rounds under this law.
Basically, we accept there’s a value to life and you don’t just kill people even if that’s what they want. And we accept the principle of patient autonomy, but see that it has limitations. We respect autonomy only if it doesn’t involve doing something active to cause the patient’s death.
Have there been changes made to the law over the past 11 years?
The law was accepted almost unanimously in the Knesset. But the ministry of health hasn’t done enough to educate either patients or physicians about the law. Our committee’s recommendations included the need for education and creating awareness, but that stuff hasn’t been done enough. We suspect the 2005 act has made a difference, but to what degree and how extensive the change has been, we don’t know. I’m consulted about this issue by hospitals all over the country. I know there are those hospitals that are interested in keeping this law.
Why were you asked to speak about this issue in Toronto 11 years after Israel’s Dying Patient Law was enacted?
There is the issue in Ontario, which I find very disturbing ethically, that Ontario doctors who don’t want to do physician-
assisted suicide must make an effective referral to another doctor that will do it. This means that if I, as a doctor, oppose participating in an act that is contrary to my ethics, I have to tell the patient, “Here’s someone who can do it for you.” This regulation doesn’t exist in any other country in the world. This infringes on the autonomy of the physician. Physicians are also people.
Why should the doctor who’s against physician-assisted suicide make the referral? Let the government make the referral. I believe this is an immoral law.
Torah in Motion wanted me to talk in Toronto about end-of-life issues in general, and particularly to talk about this aspect – this Ontario regulation – that is so disturbing to many religious physicians.
This interview has been edited and condensed for style and clarity.